Surgery for Obesity and Related Diseases ] (2015) 00–00
Has mini gastric bypass come of age?
Bruzzi et al. are to be congratulated for their contribution to the literature by describing 5-year outcomes of laparo- scopic mini gastric bypass (LMGB) with 72% follow up. This contribution is important because LMGB is growing in numbers in countries outside the United States. The authors show that their LMGB patients had good weight loss and improved quality of life at 5 years. The mean percent excess body mass index loss was 71.5% with no mortality. Notably, 82% of patients had a complete remission of type 2 diabetes. The Gastrointestinal Quality of Life Index (GIQLI) score was significantly higher in patients who were
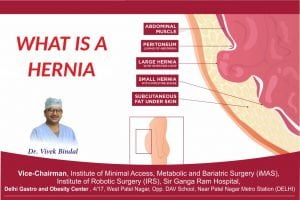
5 years post-LMGB compared with the preoperative control-group (110.3 ± 17.4 versus 92.5 ± 15.9) with an increase in physical, psychological, and social functions. These are excellent results. However, 9.6% of their patients required a surgical procedure for an early or late surgical complication. The incidence of weight loss failure was 4%, and the incidence of revision was 3.2% for excessive weight regain. This incidence of reoperation is higher than after a Roux-en-Y gastric bypass (RYGB), as pointed out by the authors themselves in their discussion [1,2]. The authors had vast experience in bariatric surgery including RYGB before performing LMBG and note that later in their LMBG experience, the reoperation rate declined, suggesting that there may be nuances that need to be learned to successfully perform and manage these patients. Although, the authors showed improved quality of life in LMGB patients, this study compares the preoperative and postoperative GIQLI scores in different sets of patients, and hence these conclu- sions need to be interpreted cautiously. Another statement that bears caution is that in the current experience, no cases of internal herniation were found with LMGB, and is a significant difference from RYGB. However, it should be noted that that the original description of internal hernia by Dr. Petersen was in patients who underwent a loop gastrojejunostomy (GJ) and which eventually resulted in mortality [3]. Thus, one should be cautious to look for internal herniation in all anastomotic bariatric procedures and mesenteric closure is recommended.
LMGB was initially described in United States in late 90s and promising results of 41,000 patients were published in
2001 [4]. It was described as a technically simpler proce- dure than the RYGB because the jejunojejunostomy (JJ) was not performed and has been frequently compared with the Mason loop gastric bypass, which was originally de- scribed in 1967 [5,6]. The Mason loop gastric bypass was eventually abandoned in favor of a Roux-en-Y configura- tion, as described by Griffen et al. [7] and modified by Torres et al. [8] for several reasons including; peritoneal contamination that could be worse in the event of anasto- motic leak from gastric/duodenal/biliary/pancreatic secre- tions and biliary reflux, which also raises the risk of developing gastric cancer in patients with a Billroth II type anastomosis [7–10]. The proponents of LMGB argue that the gastric pouch in LMGB is along the lesser curve and has better blood supply and the gastrojejunal anastomosis has lower tension thus reducing the chances of leaks. However, the potential problems of long-standing biliary reflux and associated gastric cancer still remain. For these reasons, LMGB has not been accepted widely by the bariatric community in United States, even though there is a lot of recent literature favoring LMGB, especially from Asia. Insurance reimbursements for specific procedures may play a role to this effect, but apprehensions regarding potential problems of doing away with Roux-en-Y configuration appear be a more significant factor.
The LMGB restricts stomach capacity and has a malab- sorptive/hormonal component from a considerably longer biliopancreatic limb (BPL) than the present day RYGB that has a BPL 50–75 cm in length. The longer BPL in a bilio- pancreatic diversion with or without the duodenal switch has been shown to produce better metabolic and weight loss effect without the disadvantages of a loop gastrojejunost- omy [11]. The only gain in not performing a Roux-en-Y anastomosis in LMGB is avoiding a JJ. Most bariatric surgeons will agree that creation of JJ is the easiest of the 3 steps of a gastric bypass, the other 2 being creating a gas- tric pouch and the GJ. Adding a Roux-en-Y configuration can eliminate most of disadvantages ascribed to LMGB. The surgeons who are skilled at performing a GJ should be able to perform JJ without much technical difficulty. Hence, we have to critically assess all of the experience and lessons
http://dx.doi.org/10.1016/j.soard.2014.10.001
1550-7289/r 2015 American Society for Metabolic and Bariatric Surgery. All rights reserved.
2 V. Bindal and R. Sudan / Surgery for Obesity and Related Diseases ] (2015) 00–00
learned before we subject our patients to a different procedure.
The authors have no commercial associations that might be a conflict of interest in relation to this article.
Vivek Bindal, M.S., FNB Ranjan Sudan, M.D., FACS
Department of Surgery, Duke University Medical Center
Durham, North Carolina
[1] Nandipati K, Lin E, Husain F, et al. Factors predicting the increased risk for return to the operating room in bariatric patients: a NSQIP database study. Surg Endosc 2013;27:1172–7.
[2] Sudan R, Nguyen NT, Hutter MM, Brethauer SA, Ponce J, Morton JM. Morbidity, mortality, and weight loss outcomes after reoperative bariatric surgery in the USA. J Gastrointest Surg. Epub 2014 Sep 4.
[3] Rogers AM, Ionescu AM, Pauli EM, Meier AH, Shope TR, Haluck RS. When is a Petersen’s hernia not a Petersen‘s hernia. J Am Coll Surg 2008;207:121–4.
[4] Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg 2001;11:276–80.
[5] Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am 1967;47:1345–51.
[6] Fisher BL, Buchwald H, Clark W, et al. Mini-gastric bypass controversy. Obes Surg 2001;11:773–7.
[7] Griffen WO Jr., Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg 1977;186:500–9.
[8] Torres JC, Oca CF, Garrison RN. Gastric bypass: Roux-en-Y gastrojejunostomy from the lesser curvature. South Med J 1983;76: 1217–21.
[9] Mason EE, Printen KJ, Hartford CE, Boyd WC. Optimizing results of gastric bypass. Ann Surg 1975;182:405–14.
[10] Sitarz R, Maciejewski R, Polkowski WP, Offerhaus GJ. Gastroenter- ostoma after Billroth antrectomy as a premalignant condition. WJG 2012;18:3201–6.
[11] Nelson DW, Blair KS, Martin MJ. Analysis of obesity-related outcomes and bariatric failure rates with the duodenal switch vs gastric bypass for morbid obesity. Arch Surg 2012;147:847–54.